STROKE RISK FACTORS
There are minimally-invasive procedures that can reduce the risk of a stroke: left atrial appendage occlusion (LAAO) may be an option for non-valvular AFib patients seeking an alternative to oral anticoagulants (OACs) and for patients who have had a PFO-associated stroke, closure may reduce the risk of recurrent ischemic stroke.
AF AND THE LEFT ATRIAL APPENDAGE
In patients with atrial fibrillation, the chambers of the heart contract irregularly, allowing clots to form. The left atrial appendage (LAA), a muscular pouch connected to the left atrium of the heart, can be a major site for this, with more than 90% of strokes in people with non-valvular AF (NVAF) caused by blood clots formed in the LAA.1
AF can increase the risk of stroke
90%
90% ARE CAUSED BY CLOTS FORMED IN THE LAA1
5x
5X HIGHER RISK FOR PATIENTS WITH AF2
1 in 7
1 IN 7 ARE
CAUSED BY AF3
Characteristics of strokes caused by AF3:
The challenges of oral anticoagulants
Many patients at risk of stroke want an alternative to oral anticoagulants (OACs, for example, warfarin) and non-vitamin K oral anticoagulants (NOACs).4
40%
40% DO NOT TAKE OACS (NOACS OR WARFARIN)4,5
25%
25% DISCONTINUATION
RATE (NOACS)4,6
LIFESTYLE IMPLICATIONS INCLUDE4,6:
- Significant bleeding risks
- Significant non-compliance rates
- Regular INR monitoring (warfarin)
- Food and drug interaction issues (warfarin)
- Complicates surgical procedures
- High cost (NOACs)
LAA Occlusion with the Amplatzer™ Amulet™ LAA Occluder eliminates the need for oral anticoagulants
- Transcatheter occlusion of the LAA is minimally-invasive.
- Closure rates are 98.9% with the Amplatzer™ Amulet™ LAA Occluder.7
PATENT FORAMEN OVALE (PFO)
The foramen ovale is vital for fetal circulation, when an artefact of the fetal circulatory system. Post-birth, the foramen ovale closes spontaneously in most people, but patent foramen ovale (PFO) occurs in about 25% of the population.11
Most people with a PFO are asymptomatic. But an atrial septal aneurysm may open the PFO with every heartbeat, thereby increasing the possibility for thrombus to pass from the venous to arterial system, which can cause a stroke.12
PFO closure: Behind the numbers
33%
APPROXIMATELY ONE-THIRD OF ISCHEMIC STROKES ARE DUE TO AN UNKNOWN SOURCE.13
33%
APPROXIMATELY ONE-THIRD OF ISCHEMIC STROKES ARE DUE TO AN UNKNOWN SOURCE.13
50%
Of patients with an ischemic stroke of unknown cause have a PFO12
59%
Reduction in patients 18-60 years after PFO closure compared to medical management alone14
38%
Recurrent stroke risk reduction in
patients >60 years with the Amplatzer™ Talisman™ Occluder15
Determining PFO
causation of stroke
Characteristics that are strongly associated with a causal role of PFO in an stroke of unknown cause are16:
- Atrial septal aneurysm and/or a moderate-to-severe shunt
- Atrial septal hypermobility
- PFO size
The presence of other risk factors does not exclude PFO as the causative factor, but it is more likely when patients are young and lack other risk factors. A shared decision making process between the patient and their medical team is recommended when considering PFO closure.12
RESPECT trial
long-term data17
The RESPECT trial was conducted at 69 centers across the U.S. and Canada. Alone among PFO closure studies, RESPECT included patients on anticoagulation therapy, providing a real-world cross section of patients. This trial has the most extensive follow-up data among all PFO closure studies; it spanned 13 years overall with 5,810 patient-years of safety follow-up. The RESPECT trial also revealed low rates of serious atrial fibrillation with the closure device, consistent with medical therapy.
Compelling data resulted in positive guidelines
recommending pfo closure
Long-term data from the both the RESPECT trialand REDUCE trial, as well as data from the CLOSE
trial, have revealed that with attentive patient selection, transcatheter PFO closure significantly reduces
the risk of recurrent stroke compared with medical therapy in patients with an ischemic stroke of unknown
cause—with no increased risk of serious adverse events or influence on major bleeding.17,18,19
Guidelines and recommendations
- Monitoring for Atrial Fibrillation prior to PFO Closure20 – 2022
Recommendation: In patients who have suffered a stroke that may be PFO-associated, it’s important to screen for atrial fibrillation (AF). Given the lack of clear and specific guidance available on the optimal monitoring modality and duration, an expert panel set out to provide a straightforward and personalized approach to AF detection in these patients.
The new framework provides:
- Specific monitoring timelines and modalities that account for patients with varying age and other AF risk factors
- AF monitoring ranges from 72 hours of Holter to 3 months of ICM, depending on the patient
Monitoring duration may be reduced based on presence of high-risk PFO features (i.e. large shunt and/or ASA). - Establishment of the Heart and Brain Team for PFO Closure in Stroke Patients21 – 2022
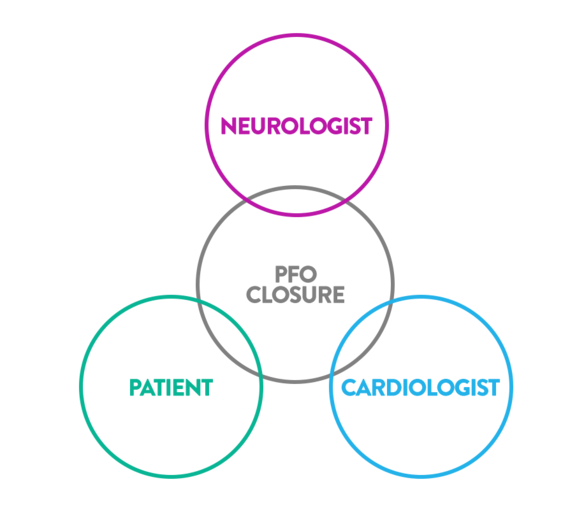
Guidelines and consensus statements emphasize the importance of multidisciplinary clinical decision-making regarding PFO closure. This multidisciplinary team – also known as the Heart and Brain Team – involves several clinical specialties, including neurology and cardiology, as well as the patient.
This review provides insights in the implementation, composition, organization and operation of a heart and brain team, as well as metrics to evaluate the team’s role.
An impactful Heart and Brain team requires upfront networking, implements an organized structure and routinely assesses effectiveness. When done well, patient waiting time and risk of loss to follow up is reduced.
- Society for Cardiovascular Angiography & Interventions (SCAI) – Guidelines for the Management of Patent Foramen Ovale22 – 2022
Recommendation: In patients between the ages of 18 and 60 with a prior PFO-associated stroke, the SCAI guideline panel recommends PFO closure rather than antiplatelet therapy alone (strong recommendation, moderate certainty of evidence).
This recommendation is independent of patient anatomy (i.e., presence of ASA, size of shunt).
A RoPE score of ≥ 7 may identify patients who are likely to receive greater benefit from PFO closure.These guidelines were developed by SCAI, with representation from the American Academy of Neurology (AAN).
- American Heart Association/American Stroke Association – Guideline for the prevention of stroke in patients with stroke and transient ischemic attack23 - 2021
Recommendation: In patients 18 to 60 years of age with a non-lacunar ischemic stroke of undetermined cause, despite a thorough evaluation and a PFO with high-risk anatomic features, it is reasonable to choose closure with a transcatheter device and long-term antiplatelet therapy over antiplatelet therapy alone for preventing recurrent stroke. (Recommendation level 2b, level of evidence B-R).
- American Academy Of Neurology – Practice advisory patent foramen ovale and secondary stroke prevention24 – 2020
Recommendation: In patients younger than 60 years with a PFO and an embolic-appearing infarct and no other mechanism of stroke identified, clinicians may recommend closure following a discussion of potential benefits (reduction of stroke recurrence) and risks (procedural complication and atrial fibrillation) (Level C).
- Asian-Pacific Consensus Statement25 - 2020
With most of the evidence on PFO closure being obtained from Caucasian patients, a consensus statement was developed by Asian-Pacific clinical experts, accounting for the specific stroke and bleeding characteristics of Asian-Pacific patients and the specific Asian-Pacific context.
Key aspects of this consensus statement include:
- Regarding indications for PFO closure, follow international/global guidelines.
- Ensure that patients with recent embolic stroke of undetermined source (ESUS) are screened for PFO, using imaging modalities that are readily available in the hospital and on which the staff is best trained and most experienced (e.g. TTE, contrast TCD, TEE, ICE). Contrast TCD is widely available in the Asian-Pacific region and may be used as a first screening tool, followed by confirmation using TEE or TTE with bubble contrast.
- ESUS patients with significant PFO should undergo PFO closure as early as possible.
It was emphasized that clinical evidence for the above aspects should be collected among Asian-Pacific patients.
- Japanese Guidance Document26 – 2019
The Japan Stroke Society, The Japanese Circulation Society and Japanese Association of Cardiovascular Intervention and Therapeutics came together to review the evidence on PFO closure and recommend the following when it comes to selecting the appropriate patient for PFO closure:
Indication criteria for percutaneous closure of PFO for the purpose of stroke recurrence prevention:
- Indispensable condition: Implementation of the intervention will be considered in case of satisfaction of all items described below:
- Patients who meet the diagnosis criteria for PFO related cryptogenic stroke
- Patients in whom antithrombotic therapy can be conducted during a certain period after percutaneous closure implementation
- Patients <60 years of age in principle
- Female patients who are not pregnant or do not want to become pregnant within a year
- Recommendation condition: Implementation of the intervention will be recommended in case of satisfaction of all aforementioned items and any items described below:
- The presence of high risk PFO in terms of function/anatomy such as:
- Large volume of shunt
- Concomitant atrial septal aneurysm (ASA)
- Concomitant Eustachian valve (EV)
- Concomitant Chiari network
- Right-left shunt found at rest (without Valsalva maneuver)
- Onset of the aforementioned type of cryptogenic stroke during appropriately conducted antithrombotic therapy.
- The presence of high risk PFO in terms of function/anatomy such as:
- Indispensable condition: Implementation of the intervention will be considered in case of satisfaction of all items described below:
- German Guidelines – cryptogenic stroke and patent foramen ovale27 – 2018
Interventional PFO closure should be performed in patients aged 16 to 60 years (after extensive neurological and cardiological diagnostic work-up) with a history of cryptogenic ischaemic stroke and patent foramen ovale, with moderate or extensive right-to-left shunt. Recommendation level A, Evidence level I.
- BMJ Rapid Recommendations28 – 2018
Among patients younger than age 60 who have had a cryptogenic ischemic stroke thought to be secondary to PFO (due to absence of other etiologies):
- Strong recommendation—among patients in whom anticoagulation is contraindicated or declined—to provide PFO closure + antiplatelet therapy, vs antiplatelet therapy alone
- Weak recommendation—among patients who are open to all options—to provide PFO closure + antiplatelet therapy vs anticoagulant therapy
- Weak recommendation—among patients in whom closure is contraindicated or declined—to provide anticoagulant therapy vs antiplatelet therapy
- European Position Paper16 – 2018
Among patients age 18-65 who have had a cryptogenic ischemic stroke cryptogenic stroke, TIA, or systemic embolism thought to be secondary to PFO due to absence of other etiologies:
- Recommend percutaneous PFO closure
- Canadian Guidelines29 – 2017
For carefully-selected patients with a recent ischemic stroke or TIA attributed to a PFO, PFO device closure plus long-term antiplatelet therapy is recommended over long-term antithrombotic therapy alone, provided all the following criteria are met: [Evidence Level A]:
- Age 18–60 years;
- The diagnosis of the index stroke event is confirmed by imaging as a nonlacunar embolic ischemic stroke or a TIA with positive neuroimaging or cortical symptoms;
- The patient has been evaluated by a neurologist or clinician with stroke expertise, and the PFO is felt to be the most likely cause for the index stroke event following a thorough etiological evaluation to exclude alternate etiologies.
The information provided is not intended for medical diagnosis or treatment or as a substitute for professional advice. Consult with a physician or qualified healthcare provider for appropriate medical advice.
MAT-2201002 v5.0 | Item approved for OUS use only.